New findings presented at EuroSpine 2025 show that using opioid pain medicines for longer than four weeks before lumbar decompression surgery increases the likelihood of ongoing use after surgery—without improving recovery.
Why Limiting Opioids Before Back Surgery Matters
Presented at EuroSpine 2025, Copenhagen
From the teams at Melbourne Orthopaedic Group and Spine & Scoliosis Research Associates Australia
The Big Picture
Opioids such as oxycodone, morphine and tramadol can help with short-term pain after injury or surgery. But when they are used for longer than a few weeks, the risks increase—tolerance, dependence and difficulty tapering off.
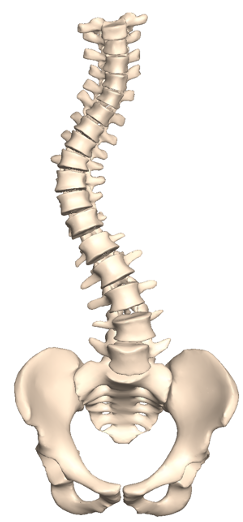
Our new study on patients undergoing lumbar decompression for lumbar spinal stenosis or disc herniation shows that taking opioids before surgery—especially for more than a month—greatly raises the chance of still using them months after surgery.
What We Studied
Who: 254 patients having one–two level lumbar decompression (77 used opioids pre-op; 177 did not).
What we measured: Opioid use in Morphine Milligram Equivalents (MME), complications, and patient-reported outcomes (function and quality of life) up to 12 months post-op.
Key Findings
- Pre-op opioids → higher risk of long-term use. Patients who used opioids before surgery were far more likely to still be taking them at 6 weeks, 3, 6 and 12 months.
- Dose tracks forward. The amount used 1–3 months before surgery strongly predicted how much was needed afterwards.
- Three times the opioid load at 6 months. Pre-op users averaged ~1,931 MME vs ~641 MME for non-users (p < 0.001).
- Function still improves. Both groups showed substantial gains in daily function and quality of life by 12 months—no significant difference between groups.
Take-home: Pre-operative opioid use doesn’t improve recovery—it mainly increases the chance of staying on opioids longer.
Why Does This Happen?
- Tolerance & sensitisation: The body adapts to opioids, so higher doses are needed for the same effect.
- Withdrawal & rebound pain: Stopping suddenly can trigger symptoms that feel like worsening pain, pushing continued use.
- Habit loops: Taking a pill becomes linked to pain relief and stress reduction, which can be hard to break.
What This Means for You
If you’re being treated for lumbar stenosis or disc herniation and considering surgery:
- Limit pre-op opioids, especially beyond 4 weeks.
- Ask for an early surgical review. Timely advice may reduce the need for escalating pain medicines before surgery.
- Use a multimodal pain plan to control symptoms without building opioid dependence.
A Safer Pain Plan (Before & After Surgery)
- Non-opioid medicines: Paracetamol/acetaminophen; short courses of anti-inflammatories (if safe for you); neuropathic agents when appropriate.
- Targeted therapies: Guided physiotherapy, core/hip strengthening, posture and pacing, heat/ice.
- Mind–body supports: Cognitive strategies for flare-ups, relaxation, sleep optimisation.
- If opioids are needed: Use the lowest dose, for the shortest time, with a clear taper plan and regular review.
Goal: pain controlled enough to move, sleep and rehabilitate—not zero pain at the cost of long-term dependence.
FAQs
Do pre-op opioids improve surgical results?
No. Functional recovery at 12 months was similar whether or not patients used opioids beforehand—but pre-op users were much more likely to still be on opioids later.
What is MME and why does it matter?
Morphine Milligram Equivalents (MME) convert different opioids into a single scale. Higher MME over time means higher exposure and greater dependence risk.
I’m already on opioids—what should I do?
Don’t stop suddenly. Talk to your surgeon or GP about a gradual taper, switching to non-opioid options and timing of surgery to help break the cycle safely.
Bottom Line
- Pre-operative opioid use > 1 month is a major warning sign for chronic post-operative use.
- You can improve your chances of getting off opioids after surgery by limiting pre-op exposure and using a multimodal plan.
- Early referral and a personalised taper can make a real difference.
Source: Summary of the e-poster presented at EuroSpine 2025, Copenhagen — “Preoperative Opioid Prescribing Prior to Lumbar Decompression Surgery Markedly Increases the Risk of Chronic Opioid Use at 6- and 12-months Postoperatively.” For more details, please speak with your care team.

For appointments or more resources, visit the News & Updates page or contact the Melbourne Orthopaedic Group care team.