Why is MIS SI Joint Fusion Considered Controversial?
- Lack of Consensus on Diagnosis: SI joint dysfunction symptoms overlap with lumbar spine and hip issues. Inconsistent diagnostic criteria raise concerns about selecting the right patients.
- Limited Long-term Data: While short-term results are promising, there is limited long-term durability data.
- Variability in Techniques and Devices: Different surgical techniques and implants yield inconsistent outcomes.
- Potential for Complications: The procedure is technically challenging and carries risks such as infection, nerve injury, implant migration, or continued pain.
- Perception of Inconsistent Outcomes: Some patients report little or no improvement, fueling debate over its overall effectiveness.
For detailed recommendations and evidence, please see the NICE Guidelines.
What Happens During MIS SI Joint Fusion Surgery?
Preparation
- Hospital Admission: Admitted on the day of surgery with required fasting as per instructions.
- Anaesthesia: Performed under general anaesthesia to ensure you are asleep and pain-free.
Surgical Approach
- Patient Positioning: Positioned prone (face down) to allow access to the SI joint.
- Incision: A small incision (typically less than 2 inches) is made over the affected hip. The gluteal muscles are gently separated with specialized retractors.
Joint Preparation & Implant Placement
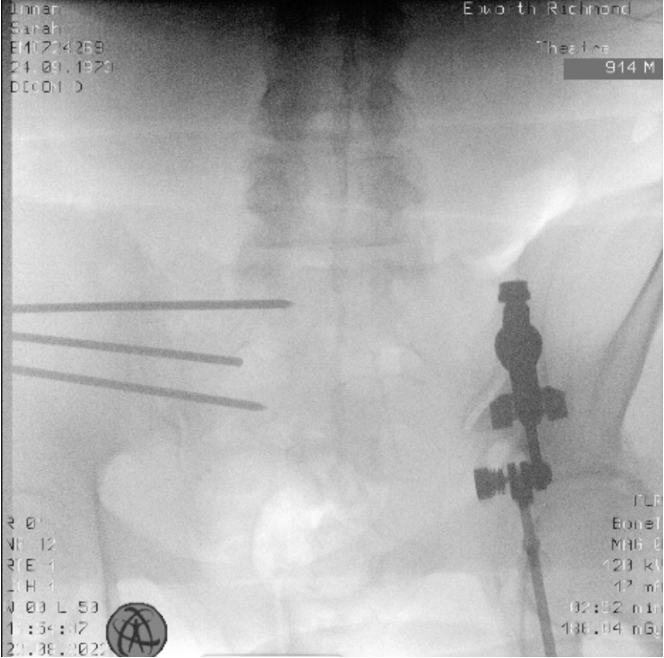
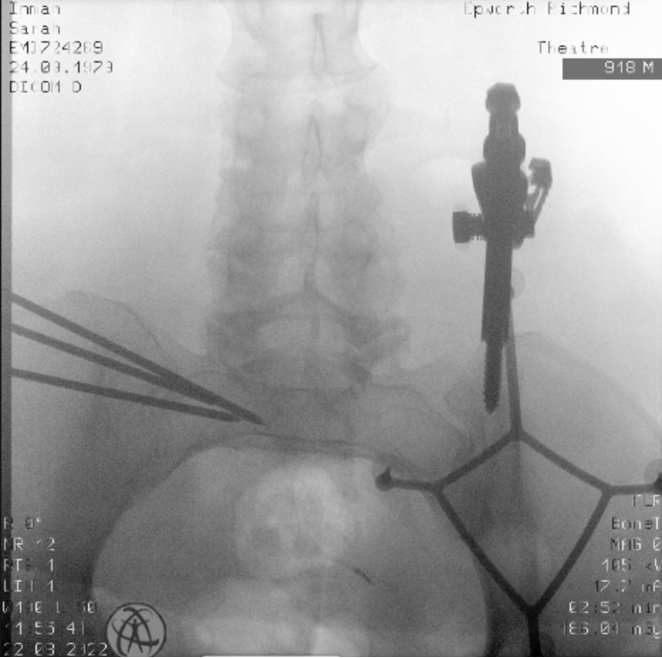
- Accessing the SI Joint: Computer navigation and fluoroscopy guide the placement of 2-3 guide-wires across the joint, with positions confirmed via X-ray.
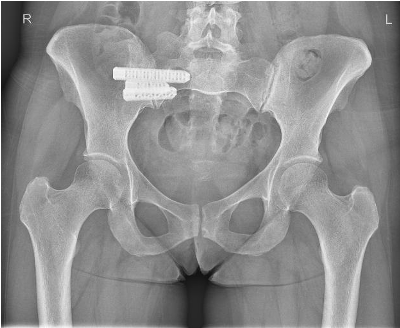
- Implant Placement: Instruments prepare the joint and adjacent bone, and definitive titanium implants are inserted. Guide-wires are then removed, and implant position is confirmed using 3D X-ray images.
Closure
- The small incision is closed with sutures or staples, and a sterile dressing is applied to protect the wound. Surrounding tissues are repositioned to minimize complications.
Intraoperative & Postoperative Imaging
Intraoperative images guide accurate implant placement.
Three Images with Caption Text Boxes
Postoperative Care and Recovery
- Hospital Stay: Most patients go home the following day, based on recovery progress.
- Pain Management: Medications and early mobilization help reduce risks such as blood clots and pneumonia.
- Rehabilitation: A tailored physiotherapy program is initiated shortly after surgery, focusing on gradual restoration of mobility and strength.
- Activity Restrictions: Crutches and partial weight-bearing are required for the first 6 weeks, with avoidance of heavy lifting, bending, and twisting for 3 months.
- Follow-Up: Regular appointments (2 weeks, 6 weeks, 3 months, 6 months, and 12 months) monitor healing and implant stability.
Risks and Complications
- Infection: A small risk exists at the surgical site.
- Bleeding: Excessive bleeding during or after surgery is possible.
- Nerve Injury: There is a risk of injury to nearby nerves, which could result in weakness, numbness, or other neurological symptoms.
- Non-Union: In some cases, the bones may not fuse as expected, potentially requiring additional surgery.
- Implant Issues: Loosening or misplacement of implants may occur.
Patient-Reported Outcomes and Results
Minimally Invasive SI Joint Fusion significantly improves function and reduces pain in most patients. For detailed outcomes and supporting literature, please click here.