Preoperative Evaluation
- Clinical Assessment: Detailed medical history and physical examination to evaluate deformity severity, symptoms, and overall health.
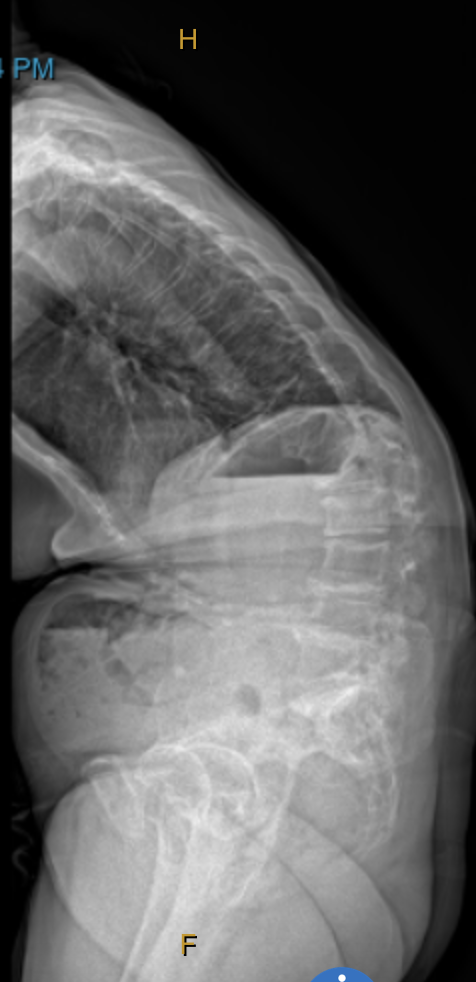
- Imaging Studies: X-rays, MRIs, and CT scans to assess spinal alignment, disc degeneration, stenosis, or nerve compression. Bone density is also evaluated.
- Functional Testing: Nerve conduction studies and other tests to determine the impact on the nervous system.
- Risk Assessment: Evaluation of fitness for surgery, including cardiac and pulmonary status, with optimization of any medical issues to reduce perioperative risks.
Surgical Planning
- Correction Strategy: The plan is tailored to the patient’s specific deformity, considering curvature type (scoliosis, kyphosis, etc.), age, bone quality, and overall health.
- Type of Surgery: Options may include spinal fusion, osteotomy, laminectomy, and implantation of rods, screws, and cages.
- Alignment Goals: The aim is to restore your specific and appropriate alignment bassed on your age and body shape.
- Neurological: Assessment of spinal cord or nerve compression requiring intervention to relieve pain and improve function.
Surgical Procedure
The surgery is performed under general anesthesia with spinal cord monitoring for safety.
- 1-Stage vs. 2-Stage Surgery: Depending on the complexity, the procedure may be done in one or two stages.
- Spinal Cord Monitoring: Small needles are placed to monitor the spinal cord and nerves in real time.
- Incision: One or several incisions are made (anterior, posterior, or combined) to access the spine.
- Instrumentation: Screws, hooks, or tapes are inserted into vertebrae using computer navigation for accurate placement.
- Decompression: Removal of parts of the vertebrae or discs may be performed to relieve pressure on the spinal cord or nerves.
- Osteotomy:Parts of the vertebra may need to be released or removed to allow larger corrections in alignment. An example is a 'Pedicle subtraction Osteotomy' (PSO).
- Correction and Stabilization: The spine is realigned and stabilized using metal rods, screws, cages, and bone grafts (from autograft, allograft, or synthetic sources).
- Intraoperative X-rays: X-rays are taken before completing the procedure to confirm proper implant placement and alignment correction.
Imaging
Risks and Complications
Adult spinal deformity correction carries a high overall complication rate. Fortunately, most complications are minor. However, significant complications can occur, including:
- Infection: Risk at the surgical site.
- Hardware Issues: Breakage or loosening of implanted hardware.
- Junctional Kyphosis or Fracture: Postural decline due to ligament failure or fracture above or below the fusion site.
- Non-union: Failure of the bones to fuse, which may require additional surgery.
- Neurological Complications: Nerve or spinal cord damage resulting in weakness or numbness.
- Blood Clots: Particularly deep vein thrombosis in the legs.
Postoperative Care
- Hospital Stay: Typically ranges from several days to a week, based on surgical complexity and recovery progress.
- Pain Management: Medications and early physical therapy help manage pain, though pain control can be challenging initially.
- Rehabilitation: Ongoing physical therapy and rehabilitation are critical; a brace may be recommended for the first 3 months.
- Follow-up: Regular visits, including X-rays, are scheduled to monitor healing and implant status.
Patient Outcomes
- Pain Relief and Function: Successful surgery can lead to significant pain relief and improved function, though some residual symptoms may persist.
- Lifestyle Modifications: Patients may need to adapt their daily activities due to reduced flexibility.
- Ongoing Monitoring: Regular follow-up is necessary, especially during the first few years post-surgery.
Patient Reported Outcomes - Adult Deformity Correction